Le test de marche de 6 minutes comme facteur prédictif de la fonction ventriculaire gauche dans un groupe de patients insuffisants cardiaques à l’Hôpital Général de Yaoundé.
Six-minute walk test as a predictor of left ventricular function in patients with chronic heart failure at the Yaounde General Hospital.
R N SEDE (1) ,A MENANGA (1,2) ,P MINTOM (2), ,HAMADOU BA (1), ,F KAZE (1,2), G ASHUNTANTANG (1,2),
E WAWO (1), S KINGUE (1,2)
RESUME
L’insuffisance cardiaque (IC) est une pathologie cardiovasculaire dans laquelle la surveillance de la fonction ventriculaire gauche est d’une importance capitale. Cependant, dans les pays en voie de développement, l’accès à l’échographie cardiaque reste assez limité.
But: Le but de cette étude était de déterminer l’utilité du test de marche de six minutes en tant que facteur prédictif de la fonction ventriculaire gauche chez des patients insuffisants cardiaques.
Méthodes: Nous avons recruté des patients ayant une IC chronique classée aux stades II et III de la NYHA. Tous les patients avaient une dysfonction systolique (fraction d’éjection ˂ 50%). Chez tous nos patients, nous avons réalisé une échographie cardiaque et un test de marche de 6 minutes à moins de 48 heures d’intervalle.
Résultats: Nous avons retrouvé une corrélation statistiquement significative entre le test de marche de six minutes et la fraction d’éjection mesurée par la méthode de Simpson (r = 0,369, p = 0,038), par la méthode de Teichholz (r = 0,489, p = 0,005) et avec la fraction de raccourcissement (r = 0,505, p = 0,004). Après analyse par régression linéaire, le test de marche de six minute (p = 0,015) et la tension artérielle systolique (p = 0,004) ressortaient comme facteurs prédictifs indépendants de la fraction d’éjection mesurée par la méthode de Simpson.
Conclusion: Il apparait que le test de marche de six minutes présente une corrélation significative avec les indices majeurs de la fonction systolique du ventricule gauche et peut prédire celle-ci.
MOTS CLES
Test de marche de six minutes, insuffisance cardiaque, fraction d’éjection, Yaoundé.
SUMMARY
Background: Heart failure (HF) is a major cardiovascular disorder in which monitoring of left ventricular function is crucial. However, availability of echocardiography machines is limited in underdeveloped countries.
Aim: The aim of this study was to investigate whether the six-minute walk test (6MWT) could be used to predict left ventricular function in patients with chronic heart failure.
Methods: We studied patients with chronic HF in the New York Heart Association (NYHA) classes II and III. All patients had systolic dysfunction (ejection fraction < 50%). They all underwent an echo-Doppler study and a 6MWT at less than 48 hours of interval.
Results: The 6MWT had statistically significant correlations with ejection fraction measured by both Simpson’s (r = 0.369, p = 0.038) and Teicholz’s methods (r= 0.489, p= 0.005) and with fractional shortening (r=0.505, p= 0.004). Multiple linear regression showed that 6MWT (p= 0.015) and systolic blood pressure (p =0.004) were independent predictors of ejection fraction measured by Simpson’s method.
Conclusion: In our study, the 6MWT correlates with major indices of left ventricular systolic function and could be used to predict and monitor left ventricular function in patients with chronic heart failure.
KEY WORDS
Six-minute walk test, heart failure, ejection fraction, predictor, Yaoundé.
1. Faculté de médecine et des sciences biomédicales/Université de Yaoundé I, Cameroun.
2. Hôpital général de Yaoundé, Cameroun
Adresse pour correspondance
NANA SEDE R.: P.O Box 5408 Yaoundé,
University of Yaounde I, Cameroon
E-mail address: Cette adresse e-mail est protégée contre les robots spammeurs. Vous devez activer le JavaScript pour la visualiser.
Tel: 00 237 99 45 41 36
INTRODUCTION
Heart failure (HF) is a major health problem which affects 23 million people worldwide [1]. This widespread condition reduces the quality and duration of life of patients such that approximately 60% of patients diagnosed with chronic heart failure (CHF) will die within 5 years of diagnosis [2]. In Africa, the increasing prevalence of heart failure places a supplementary burden on health systems, adding to that of communicable diseases.
Lack of medical personnel, medical equipment and especially lack of financial resources remain a major setback in the management of these patients in our milieu.
Left ventricular ejection fraction (LVEF) measured by echocardiography guides management and is a powerful predictor of mortality in patients with heart failure. However, following diagnosis, it is not certain that all patients will be able to benefit from an echocardiography. There is a need for accessible means of monitoring cardiac function in these patients.
The six-minute walk test (6MWT) has drawn considerable attention in this light. It is a functional test which permits objective evaluation of exercise tolerance in patients with CHF [3]. It is accessible and easy to administer [4].
Previous studies evaluating the association between the 6MWT and resting indices of cardiac function have been inconclusive [5-8]. We therefore set out to determine the usefulness of the 6MWT as a predictor of left ventricular function in patients with chronic heart failure at the Yaoundé General Hospital.
METHODOLOGY
Participant selection
This study was carried out in the Cardiology unit of the Yaoundé General Hospital.
We consecutively recruited patients with chronic heart failure at the cardiology outpatient clinic. We included all patients aged 18 years and above with chronic heart failure classified NYHA class II or III. They had left ventricular systolic dysfunction (LVEF<50%) and had given an informed consent. We excluded patients with limitation of physical activity due to factors other than exertional dyspnea and fatigue (e.g. arthritis, arthrosis, ankle/knee/hip injuries, stroke, and peripheral arterial disease). Other causes of exertional dyspnea (chronic obstructive pulmonary disease, asthma, pulmonary infection, interstitial lung disease, anaemia), pregnancy, symptomatic coronary artery disease, active infections, chronic kidney disease and mitral stenosis were also excluded.
Screening for exclusion criteria was done by consulting patients’ medical files, taking their medical history, clinical examination, and performing a full blood count, chest X-ray and a 12-lead electrocardiogram.
For the retained patients, we registered their medical treatment; we performed a clinical examination for blood pressure, pulse, weight, height, symptoms and signs of heart failure [9]. An echocardiogram was performed by the same cardiologist and a 6MWT was then carried out. The time frame from the moment of echocardiography to the 6MWT was 48 hours.
For each patient, a healthy control matched for age and body mass index was selected and an echocardiography and 6MWT done. Healthy controls here were individuals free of cardiopulmonary diseases that could limit physical activities as well as other diseases such as arthritis, arthrosis, peripheral arterial disease.
The study was approved by the National Ethics Committee.
Echocardiography
We determined left ventricular function in patients and controls using the HI-VISION HITACHI Echocardiograph.
A transthoracic echocardiogram (TTE) was performed on participants in the left lateral position with the thorax slightly raised and the arm left? folded behind the head.
The views used for evaluation of ventricular function included: long and short parasternal views (probe placed in the left 3rd or 4th parasternal space); apical view (probe placed at the apex); subcostal view (probe placed below the xyphoid process).
All echocardiography parameters were measured twice and the mean calculated.
Measurements done in M-mode echocardiography included: left ventricular internal diameter at end of diastole (LVIDd), left ventricular internal diameter at end of systole (LVIDs), interventricular septum thickness at end of diastole (IVSd), interventricular septum thickness at end of systole (IVSs), left ventricular posterior wall thickness at end of diastole (LVPWd), and left ventricular posterior wall thickness at end of systole (LVPWs). They were expressed in mm.
From these, the echocardiography machine calculated: Fractional Shortening of left ventricle (FS), End Diastolic Volume (EDV), End Systolic Volume (ESV), and Ejection Fraction by Teichholz’s Method (LVEFTM).
To estimate ejection fraction by Simpson’s Rule (LVEFSIMP), endocardial borders were traced at end of diastole and at end of systole in both apical four-chamber and apical two chamber views in two-dimensional echocardiography. The echocardiography machine then automatically evaluated ejection fraction.
Diastolic function of the left ventricle was assessed by pulsed Doppler. The pulsed Doppler sample volume was positioned at the tip of the mitral leaflets. We registered the E wave, A wave, from which the E/A ratio was calculated, and the deceleration time of E wave (DT-E). Using Tissue Doppler Imaging, we also recorded peak early diastolic annular velocity (E’). We used the Appleton classification to assess diastolic function [10]. Echocardiography also permitted us to assess the state of the valves. We evaluated mitral area using planimetry, in short parasternal view. A mitral area less than 2 cm² was considered as mitral stenosis. To assess valvular regurgitation we calculated the Effective Regurgitant Orifice Area (EROA). We considered that the regurgitation was significant, when the EROA was greater than 30 mm² for aortic regurgitation and greater than 40 mm² for mitral regurgitation [11].
Six-minute walk test
The 6MWT was carried out following the guidelines of American Thoracic Society [12]. The test was carried out on a 45 m long, straight, flat indoor corridor. The length of the corridor on which the participant walked was 30 m long and was marked every 3 m. The turnaround points were marked with bright cones.
Prior to the test, the participants were told to wear comfortable clothing and shoes appropriate for walking. They were advised against vigorous exercise within 2 hours of beginning the test.
Each participant was seated at rest in a chair next to the starting position for about 10 minutes, during which baseline blood pressure and heart rate were measured. The participants were instructed on the object of the test: to walk as far as possible on the corridor for 6 minutes. They were allowed to slow down, stop and rest when need be, but were to continue as soon as possible.
A demonstration on how to walk along the path and around the cones was done. The participant started walking as soon as the start signal was given and was told of the remaining time every minute. The participant was told to stop as soon as the six minutes had elapsed. No encouragements were given. For each lap completed, a mark was made on the worksheet.
The total distance covered was then calculated using the number of laps completed and the additional distance covered (the number of meters in the final partial lap), and rounded up to the nearest meter. At the end of the test, heart rate was again measured (end of test heart rate). Heart rate response was thus obtained by subtracting baseline heart rate from end of test heart rate.
Patients were to stop immediately if they presented with either of the following: chest pain, intolerable dyspnea, leg cramps, staggering, diaphoresis, pale or ashen appearance.
Statistical analysis
Data were analyzed using Statistical Package for the Social Sciences version 20, 0.
Descriptive statistics were presented as mean ± standard deviation for continuous variables and as percentages for categorical variables. Comparisons between groups were done using analysis of variance (ANOVA).
Bi-variate analysis between variables was perfomed using Pearson’s correlation coefficient. Linear regression was used to derive prediction equations and multiple linear regression used to identify predictors of ejection fraction.
Statistical significance using a two tailed test of significance was set at a p-value < 0.05.
RESULTS
Thirty-two patients (19 males, 13 females) with CHF and 31 controls (17 males and 14 females) entered the study. The mean age of patients was 55.9±4.4 years while that of controls was 53.87±4.26 years (p = 0.503). Heart failure was mainly of hypertensive origin (68.8%). This was followed by left heart valvulopathies in 40.6% of patients (mitral insufficiency = 25%, aortic insufficiency = 15.6%). Dilated cardiomyopathy (9.4%), peripartum cardiomyopathy (3.1%) and cardiothyreosis (3.1%) contributed to a lesser extent.
Treatment consisted mainly of diuretics (75%) and angiotensin-converting enzyme inhibitor (62.5%); 21.9% of patients were treated with beta-blockers. Duration of HF from the moment of diagnosis was less than 1 year for a great part of our population (43.8%). Minimum duration was 5 days while maximum duration was 11 years. All patients had exertional dyspnea and were either NYHA class II (68.8%) or III (31.3%).
Mean LVEFTM was 31.89±3.43% and mean LVEFSIMP was 30.60±2.89%. Fractional shortening (FS) had a mean value of 15.64±1.85%. Patients covered an average distance of 399.03±40.91 m with a minimum distance covered of 180 m and a maximum distance covered of 630 m. This was significantly lower than the distance covered by healthy subjects (547.60±28.96 m, p = 0.000). Baseline heart rate was similar in patients (77.63 ± 4.48) and controls (74.97 ± 4.58), p=0.369. End of test heart rate, however was significantly lower in patients (93.13±6.03) than in controls (108.77 ± 6.16), p = 0.001, hence a poorer heart rate response in patients (15.5 ± 4.47) than in controls (33.81±4.78), p = 0.000.
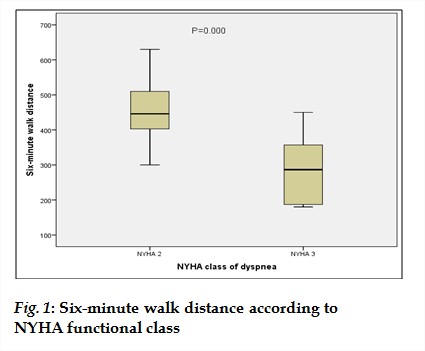
Patients in NYHA class II walked farther than patients in NYHA class III. The mean distance walked for NYHA class II was 450.86 m with a standard deviation of 86.11 m. Those in NYHA class III walked an average distance of 285 m with a standard deviation of 98.45 m. The difference was statistically significant (p= 0.000). (fig 1).
Correlations between Echocardiography variables and six-minute walk test
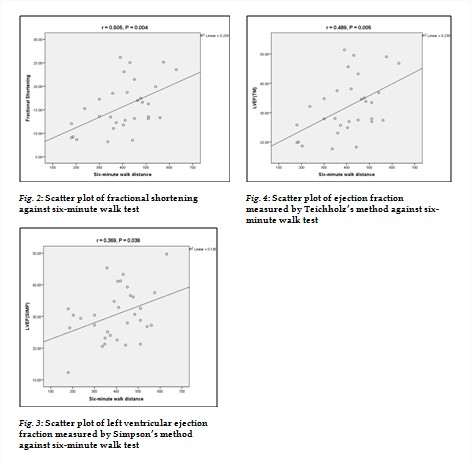
There were statistically significant correlations between FS, LVEFTM, LVEFSIMP and 6MWT. We obtained a correlation of 0.505 (p=0.004) between FS and 6MWT (fig 2). This correlation increased to 0.529 (p=0.003) when adjusting for systolic blood pressure.
The relation between 6MWT and FS was modelled using linear regression. This was significant at p=0.004. We obtained the equation:
FS = 0.022 (6MWT) + 6.759
A correlation coefficient of 0.369 with a p-value of 0.038 was obtained between LVEFSIMP and 6MWT (fig 3). On adjusting for systolic blood pressure, it increased to 0.380 (p= 0.035). The relation between 6MWT and LVEFSIMP was modeled using linear regression. This was significant at p = 0.038. We obtained the equation:
LVEFSIMP = 0.026(6MWT) + 20.214
The correlation between ejection fraction and 6MWT was better using Teichholz’s method of evaluating ejection fraction. We obtained a correlation coefficient of r=0.489 (p=0.005) which increased to r= 0.515 (p= 0.004) after adjusting for systolic blood pressure (Fig. 4). The relation between 6MWT and LVEFTM was modeled using linear regression. This was significant at p = 0.005. We obtained the equation:
LVEF(TM) = 0.040(6MWT) + 15.961
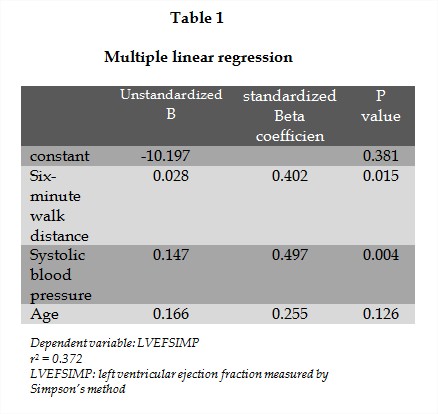
Predictors of left ventricular function
6MWT and other variables that could influence left ventricular function were fitted in a multiple linear regression model; results showed that 6MWT was an independent predictor of left ventricular function as assessed by LVEF (SIMP). Another predictor was systolic blood pressure. The model was significant at p= 0.004 (Table 1).
DISCUSSION
The aim of our study was to determine the usefulness of the 6MWT as a predictor of left ventricular function in patients with chronic heart failure.
Our study showed that the 6MWT had significant moderate to strong correlations with major indices of left ventricular systolic function as assessed by echocardiography, and was an independent predictor of left ventricular function. Hence the 6MWT can be used to predict and monitor left ventricular function in patients with heart failure.
The mean age of patients in our study was 55.91±4.4 years. This is similar to that of Ashish et al. (54.7±10 years) and that of Opasich (53±9 years) and Rostagno et al. (57.3 years) who both studied the correlation between walk performance and standard indices of cardiac function in Italy [5-7]. Berisha et al. in Kosovo had an older population (60±11 years) (8). This confirms that heart failure is mainly a disease of the aged. The six-minute walk test which is well tolerated is therefore adequate for monitoring cardiac function in these patients.
Hypertensive cardiopathy (68.8%) was the first cause of HF in our study series, followed by valvulopathies (40.6%). Similar results were obtained by Kingue et al. in 2005 [13]. They demonstrated that hypertension accounted for over half (54.49%) of cases of HF in patients followed up at the Yaoundé General Hospital. Cardiomyopathies (26.34%) and valvulopathies (24.55%) were other important aetiologies of heart failure. Ashish et al., Berisha et al. and Opasich et al. all found coronary artery disease as the main cause of heart failure. They all studied Caucasians who are known to have lower HDL cholesterol and higher frequency of tobacco use and hypercholesterolemia and therefore have a higher occurrence of coronary artery disease [14].
The mean distance covered by our patients was 399±40.91 m with a minimum distance of 180 m and a maximum distance of 630 m. This is similar to that obtained by Opasich et al. in Italy who had a mean value of 396±92 m (range= 134-686 m). Ashish et al. in India also obtained mean distance covered close to ours (384.66±115.14 m). This suggests that racial factors do not intervene in exercise tolerance in heart failure.
The controls covered a significantly higher distance (547.60±28.96 m) than the patients (399.03±40.91; P=0.000). This can be understood considering that chronic limitation of exercise tolerance is a central clinical feature in heart failure. This limitation is explained by central mechanisms with impaired regulation of blood flow to the exercising muscles; and by peripheral mechanisms with reduced muscle mass strength, reduced oxidative enzyme activity, reduced mitochondrial volume density [15].
Correlation between six-minute walk distance and left ventricular systolic function
The six-minute walk test (6MWT) presented statistically significant positive correlation with ejection fraction (EF) measured by Simpson’s method (r=0.369, P=0.038) and by Teicholz’s method (r= 0.489, P=0.005). There was also a good and significant correlation between 6MWT and fractional shortening (FS) with an r=0.505 and P= 0.004. Using a linear regression model, 6MWT stood out as an independent predictor of ejection fraction.
Thus the 6MWT correlated with the most important measures of systolic function.
Mechanisms of exercise intolerance in heart failure include both central mechanisms (among which reduced stroke volume and chronotropic response) and peripheral mechanisms (reduced muscle mass strength, decreased oxidative enzyme activity, decreased Oxidative type I fibers, decreased mitochondrial volume density) [15]. The non negligible role played by central mechanisms particularly stroke volume may explain the fact that a rise in EF is accompanied by a rise in 6MWD.
Our correlation coefficients are similar to those obtained by Ashish et al. (EF: r=0.6319, P=0.001) and Berisha et al. (EF: r=0.50, P=0.0001, FS: r=0.517, P<0.001). Rostagno et al. had a weaker but significant correlation (r=0.34, P=0.000).
Opasich et al. however, emphasize on a lack of correlation between EF and 6MWT (r=0.12, P=non significant). The difference in our results could be explained by the difference in our methods. We did a single test to evaluate 6MWT while in their study a practice test and repeat tests were done and the mean of two measurements taken as an estimate of the walking performance of each subject.
Nevertheless, in our study the 6MWT had significant moderate to strong correlations with major indices of systolic function as assessed by echocardiography and could therefore be used to predict and follow up left ventricular systolic function in patients with symptoms of heart failure.
Limitations of the study
Our study presented some weaknesses:
Our patients did not benefit from measurement of lung volumes to exclude lung diseases. However, detailed medical history, clinical examination and chest x-rays were done so as to identify those patients with potential pulmonary diseases.
Our small sample size does not permit us to generalize the results of our study.
CONCLUSION
The 6MWD correlates with major indices of cardiac function as assessed by echocardiography. It independently predicts left ventricular systolic function as assessed by ejection fraction measured by Simpson’s method.
Therefore, the 6MWT could help estimate and monitor left ventricular function in patients with chronic heart failure.
R E F E R E N C E S
1.McMurray JJ, Petrie M, Murdoch DR, Davie AP. Clinical epidemiology of heart failure: public and private health burden. Eur Heart J 1998;19:9-16.
2.McMurray JJ, Stewart S. Epidemiology, aetiology, and prognosis of heart failure. Heart 2000;83:596-602.
3.Gordon GH, Sullivan MJ, Penelope J, Thompson, Ernest LF, Stewart OP et al The 6-minute Walk; a new measure of exercise capacity in patients with chronic heart failure. Can Med Assoc J 1985;138:919-923.
4.Solway S, Brookes D, Lacasse Y, Thomas S. A Qualitative systematic overview of the measurement properties of functional walk tests used in the cardiorespiratory domain. Chest 2001;119:256-70.
5.Pramila SK, Mariya PJ, Ashish N. To correlate ejection fraction with 6 minute walked distance and quality of life in patients with left ventricular heart failure. Bombay Hospital Journal 2010; 52: 1.
6.Opasich C, Pinna GD, A Mazza, O Febo, R Riccardi, PG Riccardi et al Six-minute walking performance in patients with moderate-to severe heart failure. Is it a useful indicator in clinical practice? Eur Heart J 2001;22:488-96.
7.Rostagno C, Giorgio G, Comeglio M, Vieri B, Giuseppe O, Gian GN. Comparison of different methods of functional evaluation in patients with chronic heart failure. Eur J Heart Fail 2000;2:273-280.
8.Berisha V, Gani B, Dritero D, Haliti E, Resha B, Shperd E. Echocardiography and 6-Minute Walk Test in Left Ventricular Systolic Dysfunction. Arq Bras Cardiol 2009;92:121-34.
9.Dickstein K, Cohen-Solal A, Filippatos G, et al. Guidelines for the diagnosis and treatment of acute and chronic heart failure 2008: Task force for diagnosis and treatment of acute and chronic heart failure 2008 of the European Society of Cardiology. Eur Heat J 2008; 29: 2388-2442.
10. Appleton CP, Firstenberg MS, Garcia MJ, Thomas JD. The echodoppler evaluation of left ventricular diastolic function: A current perspective. Cardiol Clin 2000;18:513-46.
11.Zoghbi WA, Enriquez-Sarano M, Foster E. Recommendations for evaluation of the severity of native valvular regurgitation with two-dimensional and Doppler echocardiography. J Am Soc Echocardiogr 2003;16:777-802.
12.Crapo R, Enright P, Zeballos R. American Thoracic Society Statement: Guidelines for the six-minute walk test. Am J Respir Crit Care Med 2002;116:111-17.
13.Kingue S, Dzudie A, Menanga A, Akono M, Ouankou M, Muna W. A New look at adult chronic heart failure in Africa in the age of the Doppler echocardiography; experience of the medicine department at Yaoundé General Hospital. Ann Cardiol Angeiol 2005;54:276-283.
14. Onwuanyi AE, Abe O, McMahon DJ, Weil HF, Philbin EF, Francis CK, Marx H, Reed RG. Disparity in frequency of normal coronary artery in black and white patients undergoing cardiac catheterization. Ethn Dis. 2006;16:370-374.
15.Pina IL, Apstein CS, Balady GJ, Belardinelli R, Chaitman BR, Duscha BD et al. Exercise and Heart Failure: A statement from the American Heart Association Committee on Exercise, Rehabilitation, and Prevention. Circulation 2003;107:1210-25.

